“`html
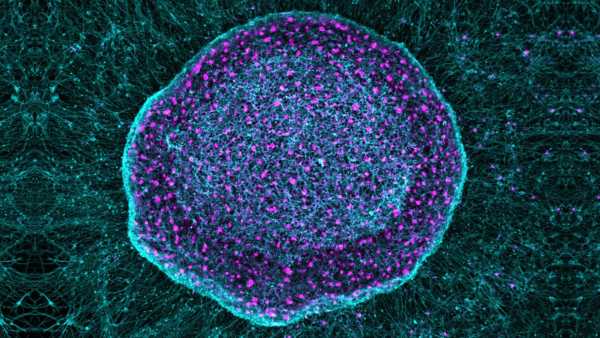
This microscopic image depicts neurons sensitive to pain, which were generated from stem cells. These particular cells are the basis of a novel “pain sponge” that captures inflammatory pain signals and impedes cartilage breakdown in arthritic mice. (Image credit: SereNeuro Therapeutics)ShareShare by:
- Copy link
- X
Share this article 0Join the conversationFollow usAdd us as a preferred source on GoogleNewsletterSubscribe to our newsletter
A tentative therapy employs unique neurons produced from stem cells to “absorb” elements that trigger pain and swelling in the arthritic knees of lab mice.
This experiment performed on mice hints that the therapy might potentially provide relief for long-lasting pain in humans, resulting from conditions such as osteoarthritis. The researchers are optimistic that the “pain sponge” may allow individuals to decrease their dependency on opioid drugs for pain management.
You may like
-
‘Mitochondrial transfer’ into nerves could alleviate chronic pain, early study hints
-

A fentanyl vaccine enters human trials in 2026 — here’s how it works
-

New drug could avert diabetes issues not addressed with blood sugar regulation, study suggests
“The likelihood that the treatment might both alleviate pain and reduce cartilage breakdown is particularly appealing for osteoarthritis,” stated Chuan-Ju Liu, an orthopedics professor at Yale University who was not linked to the investigation, to Live Science.
How the pain sponge functions
The treatment, referred to as SN101, capitalizes on human pluripotent stem cells (hPSC), which possess the ability to develop into any cell type in the body. During the study, helmed by Gabsang Lee, a neurology professor at the Johns Hopkins School of Medicine, the team modified hPSC to morph into specialized sensory neurons.
These neurons efficiently acted as an absorbent material for inflammatory pain signals. They isolated the signals before the signals were able to get transmitted to the brain and trigger pain.
According to Daniel Saragnese, a co-founder of SereNeuro Therapeutics, the biotechnology firm innovating SN101, the therapy could theoretically be applied to any form of persistent pain. However, the investigators have thus far only assessed its effectiveness for osteoarthritis, the most prevalent type of arthritis.
This progressive illness is defined by inflammation and ongoing pain that impacts the joints, predominantly the hips, knees, lower spine, and neck. It results in ache and immobility, along with inflammation that stems from the deterioration of bone, cartilage, and other tissues. There is no existing cure.
Currently, osteoarthritis symptoms are handled through modifications in lifestyle, such as physical therapy, as well as a spectrum of pain alleviating drugs, including over-the-counter and topical pain medication, opioids, and steroid injections.
Regarding neurodegenerative ailments — such as multiple sclerosis, Alzheimer’s, and Parkinson’s — scientists have been researching the usage of hPSCs to substitute or restore damaged neurons. Conversely, the researchers are adopting a different approach with SN101. The injected hPSC-derived neurons are placed at the inflammation’s location and coexist together with other neurons that sense pain, rather than taking their place.
You may like
-
‘Mitochondrial transfer’ into nerves could alleviate chronic pain, early study hints
-

A fentanyl vaccine enters human trials in 2026 — here’s how it works
-
New drug could avert diabetes issues not addressed with blood sugar regulation, study suggests
The new neurons act as biological lures, attaching to nearby inflammatory factors before the body’s original neurons can grab them.
Possible advantages of SN101
Ongoing pain, classified as pain that lasts for a minimum of three months, tends to be addressed with opioid medications that connect with receptors in the body to diminish the pain’s intensity. On the other hand, opioids result in undesirable side effects, such as queasiness and throwing up, and they carry the possibility of becoming addictive.
In spite of their drawbacks, it’s estimated that around 9% of individuals with osteoarthritis in their knees resort to opioids, potentially resulting in extreme, long-term usage. Therefore, researchers continually seek safer and more impactful techniques for handling pain.
Liu suggested that SN101, through its employment of biologically complex cells that inherently show several pain receptors, may more accurately emulate how pain and inflammation are exhibited in living tissues. This may support the extinguishing of pain right where it starts. Opioids, conversely, attach to receptors within the brain to momentarily impede painful feelings, thus failing to address the signals at the root of the pain.
“However, the study still remains in the preclinical phase,” Liu stressed.
The research must clear major milestones before being used on humans, which include official toxicology analyses, lasting safety assessments, and first-in-human clinical studies, he stated. Nonetheless, he called the therapy’s basis “groundbreaking.”
related stories
—’Breakthrough’ stem-cell patches stabilized woman’s heart as she awaited transplant
—Human knees kind of suck — here’s why we haven’t evolved better ones
—Brain signals underlying chronic pain could be ‘short-circuited,’ study suggests
The scientists noted several limits in their latest study that require investigation before SN101 can be considered safe for humans. One is the treatment’s immunogenicity — whether or not it starts a damaging immune reaction in the body. Another constraint is that human and mouse knee joints are notably different, therefore certain results from the study on arthritic mice may not be relevant to humans.
“Human joints are larger [than mouse joints], mechanically more complex, and exposed to decades of accumulated stress,” Liu pointed out. Furthermore, “pain processing and interactions between the immune system and neurons can differ greatly between mice and humans, possibly impacting the effectiveness and long-lasting nature of the treatment.”
Article Sources
Ectopic engraftment of nociceptive neurons derived from hPSCs for pain relief and joint homeostasis. Zhuolun Wang, Weixin Zhang, Ju Wang, Zhiping Wu, Xu Cao, Junmin Peng, Gabsang Lee, Xinzhong Dong. bioRxiv 2025.12.16.694733; doi: https://doi.org/10.64898/2025.12.16.694733

Payal DharLive Science Contributor
Payal Dhar (she/they) works independently as a reporter, and she focuses on science, technology, and society. They report on subjects such as AI, engineering, materials science, cybersecurity, outer space, digital games, online communities, plus any cutting-edge technology that interests them. She has written for such publications as Science News, Scientific American, Nature, Washington Post, Guardian, Chemical & Engineering News, IEEE Spectrum, among others. They are also engaged in writing science-fiction and fantasty. You can follow her @payaldhar.bluesky.social or read her work at payaldhar.contently.com.
Show More Comments
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
LogoutRead more
‘Mitochondrial transfer’ into nerves could alleviate chronic pain, early study hints

A fentanyl vaccine enters human trials in 2026 — here’s how it works
New drug could avert diabetes issues not addressed with blood sugar regulation, study suggests
‘Zombie’ cells may drive common form of epilepsy
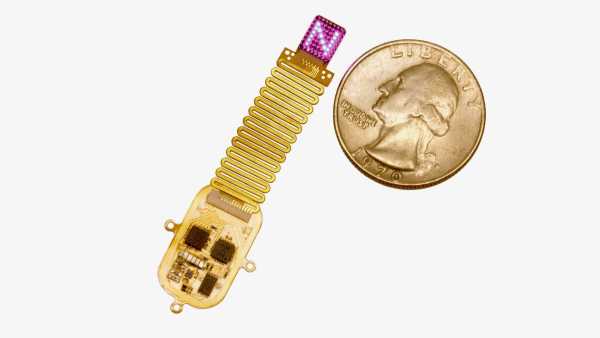
Tiny implant ‘speaks’ to the brain with LED light

Injecting anesthetic into a ‘lazy eye’ may correct it, early study suggests
Latest in Neuroscience
