“`html
Researchers are pushing back against resistance to antibiotics through novel approaches and technologies. (Image credit: wildpixel via Getty Images)ShareShare by:
- Copy link
- X
Share this article 0Join the conversationFollow usAdd us as a preferred source on GoogleNewsletterSubscribe to our newsletter
Envision visiting the clinic for a microbial ear ailment and hearing your physician state, “We have exhausted all available remedies.” It might seem extreme, but drug resistance is driving that circumstance closer to becoming a genuine possibility for a growing amount of individuals. Back in 2016, a woman residing in Nevada passed away from a microbial illness that showcased imperviousness to all 26 antibiotics then obtainable within the United States.
In the U.S. on its own, over 2.8 million drug-resistant conditions manifest per year. On a worldwide level, antimicrobial imperviousness is connected to roughly 5 million mortalities each year.
You may like
-

From genetic therapy breakthroughs to avertable disease outbreaks: The health trends destined to mold 2026
-

Newly discovered antibiotic exhibits ‘100 times’ superior efficacy versus drug-resistant microbes than its forerunner
-

Potential pandemics are a ‘certainty’ — and enhanced preparedness is crucial to impartially dispense inoculations
As bacteria displaying imperviousness proliferate, life-preserving therapeutic interventions contend with new challenges – routine ailments become harder to manage, and standard surgeries turn out to be riskier. Attenuating these jeopardies to contemporary medical procedures necessitates not only conscientious antibiotic administration and proper hygiene, but furthermore, attentiveness of the manner in which common habits impact imperviousness.
Since the commencement of antibiotics in 1910, highlighted by the advent of Salvarsan, a fabricated therapeutic substance applied to deal with syphilis, researchers have remained alert regarding imperviousness. Being a microbiologist and biochemist specializing in studying antimicrobial imperviousness, I discern four chief inclinations that will determine the means by which society tackles antibiotic imperviousness in the ensuing decade.
1. Swifter diagnostics constitute the novel first defense
For numerous decades, addressing microbial illnesses has entailed considerable knowledgeable supposition. Every time an exceptionally unwell individual reports to the hospital and doctors have yet to pinpoint the precise bacteria instigating the illness, they regularly start with a wide-spectrum antibiotic. Such therapeutic substances obliterate diverse classifications of bacteria simultaneously, which can prove life-saving — although they furthermore introduce a broad assortment of bacteria in the physique to antibiotics. Even though particular bacteria are eliminated, those that endure continue to proliferate and transmit imperviousness genes among distinct bacterial species. That unneeded susceptibility grants innocent or disconnected bacteria an opportunity to adapt and foster imperviousness.
Conversely, narrow-spectrum antibiotics zero in solely on a restricted grouping of bacteria. Doctors commonly favor such classifications of antibiotics given that they manage the ailment without disturbing bacteria which do not partake in the infection. On the other hand, it can take several days to determine the precise bacteria responsible for the infection. All through such waiting time frame, doctors frequently deem they have no alternative except to initiate wide-spectrum treatment – particularly if the individual is severely ill.

Amoxicillin constitutes a generally prescribed broad-spectrum antibiotic.
But emerging technology may expedite identification of bacterial pathogens, permitting medical analyses to be performed precisely where the individual resides instead of dispatching samples off-site and lingering for an extended duration to acquire answers. In conjunction, progressions in genomic sequencing, microfluidics, and artificial intelligence instruments are facilitating the detection of bacterial species and potent antibiotics to combat them in a matter of hours as opposed to days. Predictive instruments can even foresee imperviousness development.
To physicians, enhanced testing may bolster swifter diagnoses and impactful treatment strategies that won’t intensify imperviousness. To researchers, such instruments allude to an urgent necessity to merge diagnostics with real-time surveillance grids proficient at overseeing imperviousness patterns as they surface.
Diagnostics on their own will not resolve imperviousness, yet they bestow the precision, pace, and early notification necessitated to maintain the advantage.
You may like
-

From genetic therapy breakthroughs to avertable disease outbreaks: The health trends destined to mold 2026
-

Newly discovered antibiotic exhibits ‘100 times’ superior efficacy versus drug-resistant microbes than its forerunner
-

Potential pandemics are a ‘certainty’ — and enhanced preparedness is crucial to impartially dispense inoculations
2. Progressing beyond conventional antibiotics
Antibiotics revolutionized therapeutics in the 20th century, although counting on them singularly won’t chaperone humankind through the 21st. The inventory of innovative antibiotics stays disconcertingly scant, and the majority of therapeutic substances presently in progress bear structural resemblance to prevailing antibiotics, potentially restricting their efficacy.
The antibiotic discovery emptiness
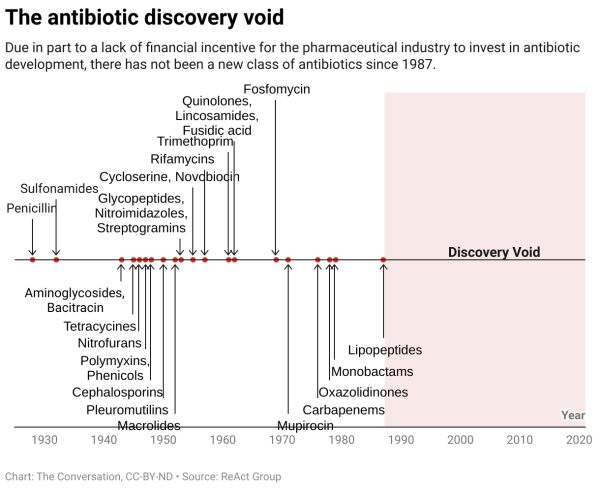
Resulting partially from a deficiency in economic enticement for the pharmaceutical sector to devote resources to antibiotic progression, there has not materialized a fresh classification of antibiotics since 1987.
To hold the edge, researchers are investing in unorthodox therapies, many of which function in fundamentally distinct methods than standard antibiotics.
One auspicious course is bacteriophage therapy, which employs viruses that selectively infect and obliterate detrimental bacteria. Additional researchers are scrutinizing microbiome-centered treatments that reinstate sound bacterial communities to monopolize pathogens.
Researchers are as well concocting CRISPR-centered antimicrobials, utilizing gene-altering instruments to precisely neutralize imperviousness genes. Novel composites like antimicrobial peptides, which perforate the membranes of bacteria to eliminate them, exhibit potential as prospective therapeutic drugs. While at the same time, scientists are structuring nanoparticle conveyance frameworks to dispatch antimicrobials directly to infection sites while diminishing adverse effects.
Outside of medication, scientists are scrutinizing ecological involvements to curtail the migration of imperviousness genes across soil, wastewater, and plastics, as well as spanning waterways and pivotal environmental reservoirs.
Numerous of such possibilities continue to exist in preliminary phases, and bacteria could potentially evolve to circumvent them. Although, these innovations mirror a potent conversion: As opposed to gambling on discovering a solitary antibiotic to manage imperviousness, researchers are assembling a more varied and resilient toolbox to combat antibiotic-resistant pathogenic bacteria.
3. Antimicrobial imperviousness outside of health facilities
Antibiotic imperviousness does not merely proliferate within health facilities. It transits through individuals, fauna, crops, wastewater, soil, and worldwide commercial networks. This broader perspective that factors the tenets of One Health into consideration is indispensable for comprehending the manner in which imperviousness genes traverse ecosystems.
Researchers progressively recognize environmental and agricultural elements as principal instigators of imperviousness, equivalent to abuse of antibiotics within the clinic. These involve the manner in which antibiotics utilized in animal husbandry can spawn resistant bacteria that propagate to individuals; the manner in which imperviousness genes present in wastewater can persist through treatment systems and infiltrate rivers and soil; and the manner in which farms, sewage facilities, and other environmental hot spots transform into hubs where imperviousness proliferates swiftly. Moreover, global commuting hastens the conveyance of resistant bacteria across continents in a matter of hours.
The Trouble with Antibiotics (full documentary) | FRONTLINE – YouTube

Watch On
Jointly, these forces reveal that antibiotic imperviousness isn’t solely a concern for health facilities – it’s an ecological and societal predicament. To researchers, this signifies structuring resolutions that traverse disciplines, consolidating microbiology, ecology, engineering, agriculture, and public health.
4. Policies pertaining to existing treatments in the future
Pharmaceutical firms incur losses fostering innovative antibiotics. Since innovative antibiotics are utilized sparingly to conserve their potency, firms commonly vend too few amounts to recoup growth expenditures even subsequent to Food and Drug Administration endorsement of such drugs. Multiple antibiotic firms have undergone bankruptcy for this particular reason.
To motivate antibiotic innovation, the U.S. contemplates major policy modifications like the PASTEUR Act. This bipartisan measure suggests instating a subscription-oriented payment scheme that would allow the federal administration to expend up to US$3 billion to remunerate drug manufacturers across a span of five to 10 years for admission to critical antibiotics instead of remunerating per pill.
Global health establishments, encompassing Médecins Sans Frontières (Doctors Without Borders), admonish that the measure ought to encompass stronger pledges to stewardship and impartial admission.
Still, the measure embodies one of the most noteworthy policy suggestions pertaining to antimicrobial imperviousness in U.S. history and could ascertain which antibiotics exist in the future.
The future of antibiotic imperviousness
Antibiotic imperviousness is at times depicted as an inescapable calamity. Although I contend the actuality is more auspicious: Society is penetrating an epoch of smarter diagnostics, inventive therapies, ecosystem-level strategies, and policy reforms geared towards rebuilding the antibiotic inventory in addition to tending to stewardship.
To the public, this indicates superior instruments and stronger frameworks of protection. To researchers and policymakers, it signifies collaborating in innovative manners.
The question at present isn’t whether resolutions to antibiotic imperviousness materialize – it’s whether society will function expeditiously enough to employ them.
This revised article is republished from The Conversation beneath a Creative Commons license. Read the original article.

André O. HudsonDean of the College of Science, Professor of Biochemistry, Rochester Institute of Technology
The fundamental topics of inquiry within the Hudson laboratory are engaged in biochemistry and microbiology. With greater specificity, concerning the domains of amino acid metabolism, structural investigations of enzymes participating in amino acid and bacterial peptidoglycan metabolism that embody supposed targets for antibiotic progression, coupled with the isolation, detection, and genomic depiction of plant-linked bacteria. Dr. Hudson has garnered roughly $3 million in federal/state subsidized grants and contracts acting as PI and/or CoPI courtesy of the NIH, NSF, Bayer Corporation, Sweetwater Energy, and Natcore Technology. Dr. Hudson has released beyond 75 peer-evaluated publications.
Dr. Hudson presents as a remarkably respected and greatly admired educator. His educational inputs are considerable most notably during the shift to semesters wherein he revamped each of the courses he instructs. Dr. Hudson has mentored and enveloped numerous students within research and has disseminated within peer-evaluated journals alongside a multitude of them. A profusion of his students has proceeded onward to pursue advanced inquiry at prestigious establishments. Dr. Hudson entered the RIT faculty back in 2008, subsequent to a post-doctoral fellowship situated at Rutgers University. He acquired his B.S. (2000) in Biology hailing from Virginia Union University, Richmond, VA., and his Ph.D. (2006) in Plant Biochemistry from Rutgers University.
Show More Comments
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
LogoutRead more

From genetic therapy breakthroughs to avertable disease outbreaks: The health trends destined to mold 2026

Newly discovered antibiotic exhibits ‘100 times’ superior efficacy versus drug-resistant microbes than its forerunner
