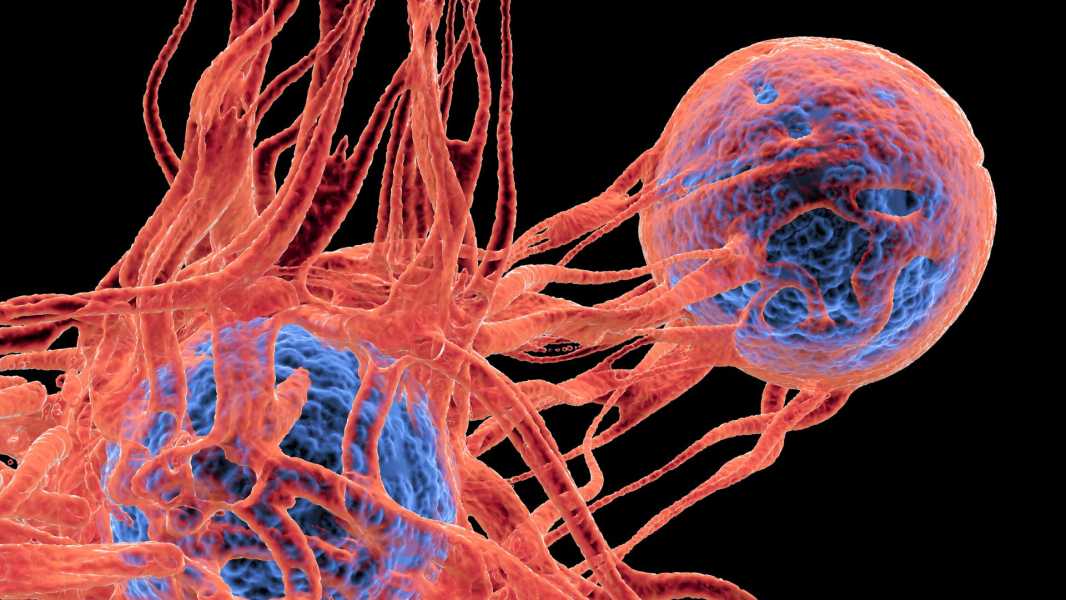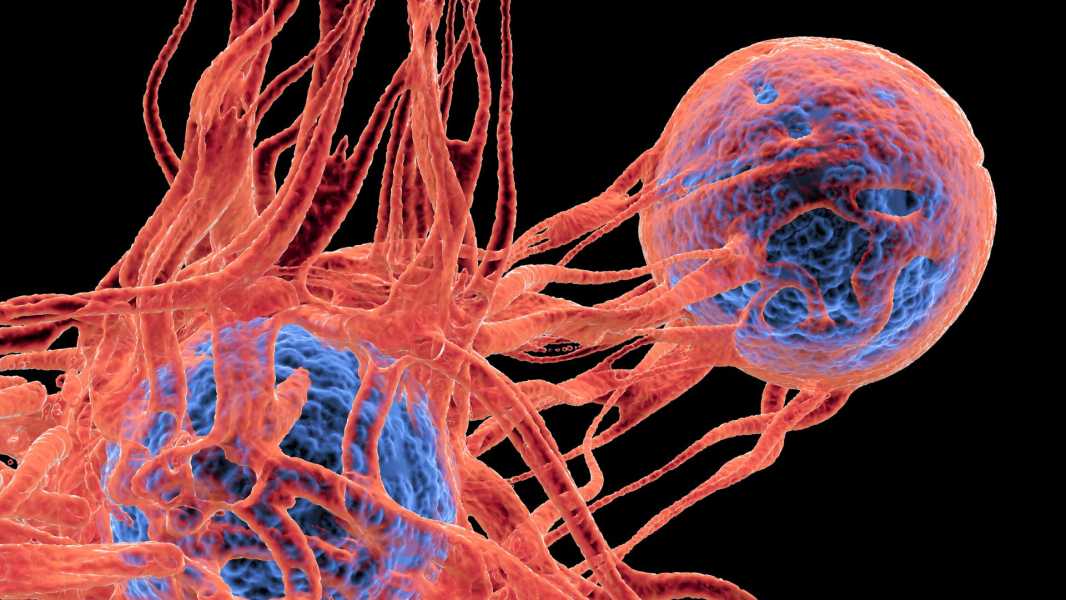
A blood test that detects cancer DNA could help determine whether a patient's dangerous skin cancer is likely to recur after surgery. (Image credit: ALFRED PASIEKA/SCIENCE PHOTO LIBRARY via Getty Images)
A simple blood test can determine who is at higher risk of skin cancer coming back after a tumor is removed.
The test can detect fragments of tumour DNA using a simple blood draw to identify stage III melanoma – a metastatic form of the most dangerous skin cancer – that cannot be diagnosed with a CT scan. While the test is not perfect, it can help identify patients who need intensive treatment because their cancer is at high risk of returning.
“We envision the test being used to monitor patients over time (perhaps every month or several months for the first 1-3 years after surgery) for early detection of melanoma recurrence,” senior study author Dr. David Polsky, a dermatologist-oncologist at NYU Grossman School of Medicine, told Live Science in an email.
Polsky added that if the test shows the presence of tumor DNA, the doctor may decide to use more advanced imaging techniques to look for small, hard-to-find tumors or move to more aggressive treatment using a combination of anti-cancer drugs instead of just one.
Melanoma is a cancer of the melanocytes, a type of pigmented skin cell. It accounts for only 1% of all skin cancers, but causes the most skin cancer deaths because it can quickly spread to other organs, or metastasize. Early detection is one of the most effective ways to improve your chances of survival.
Polsky and his team focused on stage III melanoma, which is melanoma that has spread to nearby lymph nodes, where immune cells are found and stored. Doctors perform surgery to remove as many cancer cells as possible before beginning treatment to kill any remaining tumor cells.
Patients then undergo CT scans to check for signs of recurrence, but some have tiny deposits of melanoma that aren’t large enough to be detected by CT. To find these deposits early, Polsky and his team turned to circulating tumor DNA, or ctDNA. These are fragments of DNA that tumor cells shed as part of their normal life cycle. These fragments circulate in plasma, the liquid part of the blood, and can be detected by characteristic mutations unique to the cancer.
As part of a larger clinical trial of the cancer drug combination, the research team looked at blood samples from 597 patients who had recently undergone surgery. Participants also gave control blood samples at three, six, nine and 12 months after starting treatment or taking a placebo.
Immediately after surgery, 13% of patients had detectable ctDNA in their blood plasma. The researchers found that all of these patients had cancer recurrence. Patients were also more likely to have melanoma recurrence if their ctDNA increased during follow-up testing or remained consistently high during testing.
The presence of ctDNA predicted the cancer would return 100% of the time; no one with a positive test avoided melanoma recurrence. However, the absence of ctDNA did not guarantee that patients were out of danger. A negative test was correct 71% of the time, predicting that a person’s cancer would not return. However, some patients with undetectable ctDNA still had a recurrence.
“The tests are very accurate when they are positive, but not so reliable when they are negative,” Polsky said.
The study’s findings were published April 15 in The Lancet Oncology. The next step, Polsky said, is to bring the test into a clinical molecular pathology lab, where it could be used to guide treatment decisions. The trial could also show whether using the blood test leads to better outcomes than not using it — a measure called “clinical utility.”
“Confirming the clinical utility of the test will be a significant advance in patient care
Sourse: www.livescience.com