
Why do certain allergies disappear over time, while others persist indefinitely? Current investigations are starting to solve the puzzle.(Image credit: mladenbalinovac via Getty Images)ShareShare by:
- Copy link
- X
Share this articleJoin the conversationFollow usAdd us as a preferred source on GoogleNewsletterSubscribe to our newsletter
Pleasant weather will soon favor the U.S., taking the place of winter’s abbreviated, chilly days — however, it will likewise bring about a flood of recurrent springtime sensitivities. Could a time come when sensitivities are an ancient memory?
Surprisingly, regarding that aspect, there’s a ray of optimism.
Researchers recently made strides toward clarifying why specific sensitivities might last for a lifetime while others lessen. As it turns out, the constancy of sensitivities may be associated with a distinctive kind of immune cell — and in due course, by adapting or eradicating these cells, scientists might, in theory, assist in making individuals’ sensitivities less bothersome or even eliminate them entirely.
You may like
-
A ‘functional cure’ for HIV may be in reach, early trials suggest
-

Aging and inflammation may not go hand in hand, study suggests
-
Chemo hurts both cancerous and healthy cells. But scientists think nanoparticles could help fix that.
Sensitivities have perplexed scientists for a while — researchers don’t completely comprehend why sensitivities impact certain individuals and not others, or why sensitivities surface in the first place. Prior investigations have revealed that the kind of antibody most often associated with sensitivities is created by cells that don’t remain for very long in the body, which makes lifelong sensitivities more challenging to explain.
Two current investigations, released consecutively in the journal Science Translational Medicine, might contribute toward resolving that puzzle. The investigations, one of which examined children with sensitivities and the other adults, depicted a distinctive kind of immune cell that hasn’t formerly been associated with sensitivities.
These cells regularly generate a kind of antibody not associated with sensitivities, referred to as immunoglobulin G (IgG). However, a fraction of these cells, in fact, convert to generating a sensitivity-related antibody referred to as immunoglobulin E (IgE) when faced with an allergen, be it pollen, pet fur, or peanuts.
IgE is typically generated by fleeting plasma cells, which produce antibodies as an immediate and short-term defensive measure for the body. These antibodies are believed to contribute to combatting parasites, for example, but with sensitivities, they pursue innocuous proteins instead.
The recently depicted cells are a kind of memory B cell, which generally recall viruses and bacteria and expel IgG when those invaders surface. But now, scientists have discovered a fraction of memory B cells that recall allergens and can generate IgE. These cells aren’t fleeting like plasma cells; rather, they linger in the body for an undefined duration — numerous years, or possibly a person’s entire life.
The new investigation could prove useful in formulating novel treatments or evaluations for sensitivities — for example, to evaluate if a childhood sensitivity is prone to remain into adulthood, as stated by the study researchers.
You may like
-
A ‘functional cure’ for HIV may be in reach, early trials suggest
-

Aging and inflammation may not go hand in hand, study suggests
-
Chemo hurts both cancerous and healthy cells. But scientists think nanoparticles could help fix that.
“These cells might be considered as a kind of [biological indicator] for susceptibility to sensitivities or sensitivity endurance,” expressed Maria Curotto De Lafaille, a professor of pediatrics and of immunology and sensitivity at the Icahn School of Medicine at Mount Sinai Hospital in New York and senior author of the investigation on children.
That investigation centered on children with peanut sensitivities and analyzed blood samples from 58 children who are sensitive to peanuts and 13 who are not. The second investigation analyzed a smaller number of blood samples from adults with an assortment of sensitivities, including six with a birch-pollen sensitivity, four with a dust-mite sensitivity, and 11 with peanut sensitivities.
Levoit Core 600S

We’ve assessed all the leading air purifiers for sensitivities and consider the Levoit Core 600S the optimum overall. It functions quietly and unobtrusively, is simple to manage by way of the app, and is robust. Read our full Levoit Core 600S review for more.
While each of the children with sensitivities abstained from consuming peanuts, participants in the adult investigation with birch-pollen sensitivities contributed blood samples prior to and following commencement of an immunotherapy treatment for their sensitivities. This treatment is intended to desensitize the immune system by presenting patients with a modest amount of allergen and then steadily raising the dosage with time.
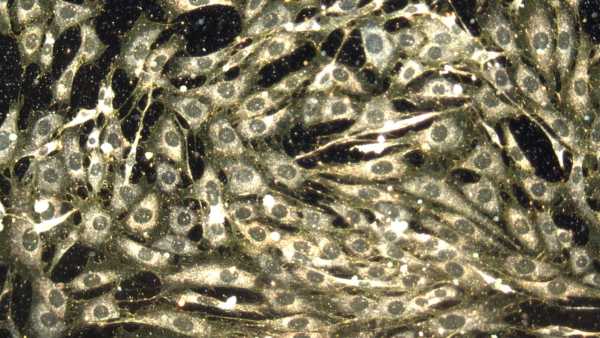
Both investigations searched for indications that memory B cells could convert to generating IgE after being exposed to allergens. For instance, researchers examining samples from children searched for B memory cells with a particular kind of receptor, or component of the antibody that allows it to attach to particular proteins. This receptor is more prevalent in individuals with eczema and asthma, two inflammatory ailments that frequently coincide with sensitivities, than in individuals without the ailments.
The two investigations pinpointed the same kind of memory B cell in individuals with sensitivities, although notably, earlier investigation had revealed similar cells in animals and in individuals with asthma and eczema.
The cells “directly produce IgE antibodies, the kind that makes us sensitive,” Joshua Koenig, an assistant professor of medicine at McMaster University in Canada and the first author of the paper focused on adults, informed Live Science via email. “They’re truly the long-term memory store of sensitivity.”
The investigation is part of “an important area of study, and the key to understanding the persistence of diseases that are caused by antibodies, like allergies,” Dr. Sarita Patil, an assistant professor of sensitivity and immunology at Harvard Medical School who was not involved in the studies, communicated to Live Science via email.
Both investigations were restricted by encompassing a small quantity of participants. Future investigation could examine how immunotherapy for peanut sensitivities influences the recently depicted cells and the antibodies they discharge. It’s understood that the immunotherapy lessens people’s allergen-specific IgE levels over time, but the impact on these memory B cells is uncertain.
RELATED STORIES
—What triggers metal sensitivities?
—Can you genuinely be sensitive to the sun?
—Sensitivity compared to cold: which is it?
Additional future investigation could observe if the behavior of these cells alters with time, notably in children, who occasionally outgrow their sensitivities.
Comprehending why sensitivities persist could one day assist scientists in eradicating or adapting these sensitivity-specific cells so they cease to generate IgE and activate an immune reaction, Lafaille stated. Put differently, investigations building on this investigation might one day assist in mitigating the impact of sensitivities or even curing them.
Editor’s note: This story was updated on April 12, 2024. It was first published on Feb. 16, 2024.
This article is for informational purposes exclusively and isn’t intended to provide medical counsel.
Do you ever wonder why some individuals develop muscle more readily than others or why freckles emerge in sunlight? Forward your inquiries regarding how the human body operates to [email protected] using the subject line “Health Desk Q,” and you may see your question addressed on the website!

Rebecca SohnSocial Links NavigationLive Science Contributor
Rebecca Sohn is a self-employed science journalist. She reports on a diverse array of science, health, and ecological subjects and is particularly intrigued by the ways science shapes individuals’ lives. She’s functioned as an intern at CalMatters and STAT, as well as a science fellow at Mashable. Rebecca, an inhabitant of the Boston vicinity, studied English literature and minored in music at Skidmore College in Upstate New York, and afterward studied science journalism at New York University.
Read more
A ‘functional cure’ for HIV may be in reach, early trials suggest

Aging and inflammation may not go hand in hand, study suggests
Chemo hurts both cancerous and healthy cells. But scientists think nanoparticles could help fix that.

Insomnia and anxiety come with a weaker immune system — a new study starts to unravel why

‘As if a shudder ran from its brain to its body’: The neuroscientists that learned to control memories in rodents
