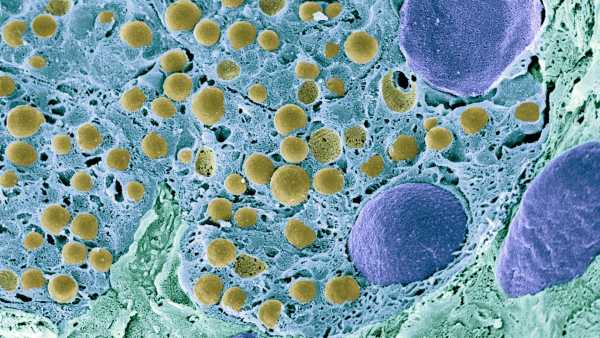
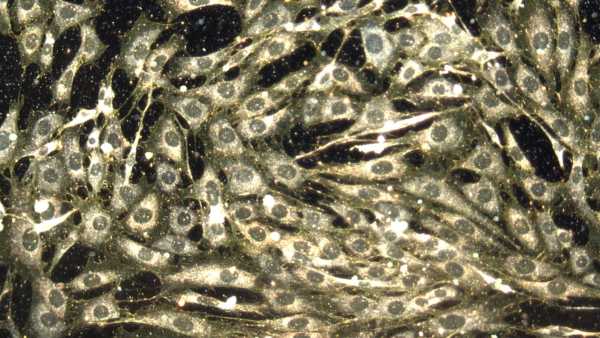
A scanning electron microscope visualization of pancreatic cells.(Image credit: Science Photo Library – STEVE GSCHMEISSNER. via Getty Images)ShareShare by:
- Duplicate link
- X
Share this articleJoin the discussionFollow usInclude us as a favored source on GoogleNewsletterEnroll in our newsletter
Chinese scientists have, for the first time, altered a woman’s adipose cells to transform them into insulin-creating pancreatic cells, which subsequently reversed her type 1 diabetes.
This achievement bolsters the rising collection of proof that altered stem cells might someday be used to manage or treat the persistent ailment. The patient involved in the current research still has no requirement for injected insulin a full year following her procedure.
You may like
-

What constitutes type 5 diabetes? Emerging understanding of the ailment is gaining recognition
-

A novel medicine might avert diabetes complications that aren’t corrected by glucose regulation, a study suggests
-
Eradicating ‘zombie cells’ inside blood vessels could be crucial for managing diabetes, initial research indicates
Insulin serves as the biochemical gateway, enabling glucose molecules to depart from the bloodstream and permeate into cells, where they can be used for energy. However, in type 1 diabetes, the immune response decimates the body’s insulin-generating cells, which are nestled within larger “mini-organs” in the pancreas, referred to as islets.
In the absence of insulin, cells undergo fuel deprivation while blood glucose levels escalate. In serious cases, individuals may die as the body generates acidic substances, known as ketones, in an effort to supply enough energy for cell survival.
In the recent study, which appeared Thursday (October 31) in the publication Cell, scientists harvested adipose cells from a type 1 diabetes patient and employed chemicals to revert them into “pluripotent” stem cells, implying they had the ability to develop into any cell type.
After returning the cells to this state, the researchers used chemical means to prompt them to transform into islet cells. These fresh islet cells were then introduced into the patient’s abdominal cavity.
Before receiving this experimental therapy, the patient experienced difficulty managing her glucose levels, spending less than 50% of her time in a “target” range of healthy blood glucose, as reported by study head Hongkui Deng, a scientist at the Peking-Tsinghua Center for Life Sciences at Peking University in Beijing. After the patient’s cell transplant, her time in the intended zone “increased to over 98%,” Deng mentioned to Live Science via email.
By the 75th day post-transplant, the patient no longer had a need to inject insulin to maintain glucose levels.
You may like
-

What constitutes type 5 diabetes? Emerging understanding of the ailment is gaining recognition
-
A novel medicine might avert diabetes complications that aren’t corrected by glucose regulation, a study suggests
-
Eradicating ‘zombie cells’ inside blood vessels could be crucial for managing diabetes, initial research indicates
“The pace at which the patient demonstrated a reversal of diabetes and achieved insulin independence following transplantation was noteworthy,” Deng noted. “This observation highlighted the considerable capacity of this treatment approach.”.
Transplanting islet cells into individuals isn’t a novel approach. For the past 30 years, researchers have extracted islets from donated bodies and then transferred these cells into the livers of type 1 diabetes patients. However, the number of available donors is limited, and transplant recipients must ingest potent pharmaceuticals indefinitely to suppress the immune system and prevent the rejection of their new mini-organs. Consequently, only patients requiring other transplants, such as kidney or liver transplants, typically receive islet cells from donors.
The patient in the recent study was similar in this regard. She had previously undergone a liver transplant and, as such, was taking strong immunosuppressants. Even so, the innovative form of islet transplant she received signifies progress: Unlike cells from donated bodies, stem cells offer an essentially boundless reservoir of fresh islets.
The cells introduced into the abdomen performed better than those often implanted in the liver, exhibiting “markedly enhanced insulin secretion,” Deng pointed out. Moreover, the abdominal region is easily accessible and can be scanned utilizing MRI. That means that the implanted cells can be readily monitored for safety and extracted should they begin to malfunction, he added.
RELATED STORIES
—A recently discovered ‘death receptor’ may aid in the progression of type 1 diabetes
—For the first time, a baby’s heart defect is successfully addressed with injected stem cells
—The initial woman to receive a stem cell transplant to eliminate HIV is still virus-free after 5 years
The current research adds to the growing array of proof that islets derived from stem cells may reverse type 1 diabetes, at least temporarily. For example, Vertex Pharmaceuticals is creating islets derived from embryonic stem cells and has shown that these cells have the potential to normalize glucose levels, at least in the few patients tested thus far.
Although the novel stem cell treatment may not encounter the typical risks related to organ rejection, the transplanted islets might still be singled out for destruction by the immune system. For this therapy to be suited to a broader range of type 1 diabetes patients, researchers must identify a method to render stem cell transplants undetectable to the immune system, without the need for potent immunosuppressants.

Tia GhoseSocial Links NavigationEditor-in-Chief (Premium)
Tia functions as editor-in-chief (premium), formerly holding positions as managing editor and senior writer for Live Science. Her contributions have been featured in Scientific American, Wired.com, Science News, and various other publications. She possesses a master’s degree in bioengineering from the University of Washington, a graduate certification in science writing from UC Santa Cruz, and a bachelor’s degree in mechanical engineering from the University of Texas at Austin. Tia was part of a team at the Milwaukee Journal Sentinel that released the Empty Cradles series on preterm births, receiving various accolades, including the 2012 Casey Medal for Meritorious Journalism.
Read more

What constitutes type 5 diabetes? Emerging understanding of the ailment is gaining recognition
A novel medicine might avert diabetes complications that aren’t corrected by glucose regulation, a study suggests

Eradicating ‘zombie cells’ inside blood vessels could be crucial for managing diabetes, initial research indicates
An HIV ‘functional cure’ may be within reach, new trials propose
An experimental mRNA-based therapy combats immune cell aging in rodents
Chemotherapy injures cancerous and healthy cells alike. However, scientists believe that nanoparticles could assist in rectifying this.
Latest in Diabetes
Eradicating ‘zombie cells’ inside blood vessels could be crucial for managing diabetes, initial research indicates
