
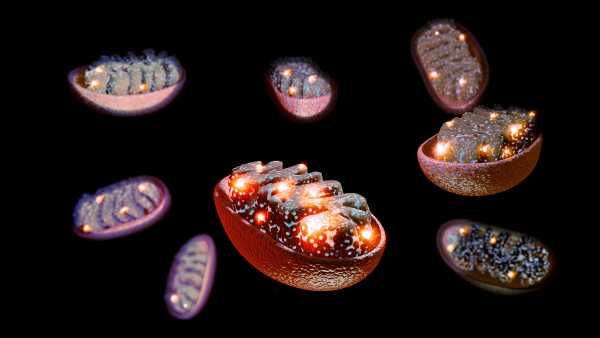
Insufficient sleep kicks off a signaling process from the brain to the digestive tract, which harms intestinal stem cells and curtails their potential for renewal.(Image credit: SEBASTIAN KAULITZKI/SCIENCE PHOTO LIBRARY via Getty Images)
- Copy link
- X
Share this article 0Join the conversationFollow usAdd us as a preferred source on GoogleNewsletterLive ScienceGet the Live Science Newsletter
Receive the most captivating discoveries from across the globe delivered directly to your inbox.
Become a Member in Seconds
Gain immediate entry to member-only perks.
Contact me with news and offers from other Future brandsReceive email from us on behalf of our trusted partners or sponsorsBy submitting your information you agree to the Terms & Conditions and Privacy Policy and are aged 16 or over.
You are now subscribed
You’ve successfully subscribed to our newsletter
Interested in subscribing to additional newsletters?

Delivered DailyDaily Newsletter
Register to get the newest finds, innovative investigations, and enthralling developments that affect both you and the world around you, straight to your inbox.
Signup +

Once a weekLife’s Little Mysteries
Indulge your curiosity with a unique mystery each week, deciphered through science and sent directly to your inbox before it’s revealed elsewhere.
Signup +

Once a weekHow It Works
Join our complimentary science and technology bulletin for your regular dose of captivating pieces, brief quizzes, amazing visuals, and more
Signup +

Delivered dailySpace.com Newsletter
Get the newest space updates, rocket launch developments, stargazing opportunities and much more!
Signup +

Once a monthWatch This Space
Join our monthly entertainment newsletter to stay informed on our reporting of the recent science fiction and space films, TV shows, games and literary works.
Signup +

Once a weekNight Sky This Week
Uncover this week’s essential night sky happenings, lunar phases, and striking astrophotography. Subscribe to our stargazing bulletin and explore the cosmos alongside us!
Signup +Join the club
Gain complete access to premium articles, unique features and an expanding collection of member incentives.
Explore An account already exists for this email address, please log in.Subscribe to our newsletter
A singular night or two of deficient sleep has consequences beyond causing weariness — it can also negatively impact stem cells inside the gut, rendering the organ vulnerable to disorders involving inflammation, according to a study on mice.
The present investigation showed that a deficit of sleep impedes the operation of intestinal stem cells in manners that could heighten susceptibility to inflammatory bowel disease (IBD), which encompasses ulcerative colitis and Crohn’s disease.
You may like
-

Initial studies suggest reasons for why women undergo sharper gut pain than men
-

A new investigation begins to decipher why insomnia and anxiety accompany a weakened immune response
-
Early study suggests that eliminating ‘zombie cells’ inside blood vessels could be vital to treating diabetes
“We currently have proof indicating that sleep is not simply [important] for the brain, but also for general well-being,” stated Dragana Rogulja, a Harvard Medical School neuroscientist who was not involved with the investigation, to Live Science.
It’s estimated that insomnia impacts 10% of grown-ups across the globe. In addition to playing havoc with individual’s daily performance, continual disruptions in sleep patterns are correlated with an elevated likelihood of contracting numerous enduring ailments, such as IBD, diabetes, elevated arterial tension and substantial depressive ailments.
Among those diagnosed with IBD, in excess of 75% report enduring disrupted sleep. Within a research project involving over 1,200 participants whose IBD was exhibiting remission, those who slept poorly faced twice the likelihood of relapse as opposed to fully-rested participants with the same ailment. Nevertheless, the preponderance of investigations on sleep disturbances emphasize the brain; thus, it has been largely indefinite as to how such disruptions may impact other bodily organs, such as the gut.
To ascertain the means through which the brain under sleep deprivation influences the bowels, the investigators concentrated on intestinal stem cells, which assume central roles in maintaining the well-being of the gut — most specifically, the robustness of the organ’s lining. They induced sleep deprivation among mice for a period of two days, after which they noted that their intestines exhibited indications of oxidative pressure. These mice featured approximately half the stem cell quantity in comparison to the guts of mice that were adequately rested, along with a lessened capacity to rejuvenate subsequent to suffering damage.
“This vividly illustrated the rate and intensity at which sleep disruption can damage the gut,” Zhengquan Yu, co-author of the investigation and molecular biologist at China Agricultural University, relayed to Live Science.
A more thorough examination of the molecular alterations occurring inside the intestines unveiled a correlation between sleep deprivation and a serotonin increase within the guts of the test mice. Serotonin plays a critical part in triggering the gut for release of digestive fluids and governing the muscular contractions that propel food along within the system. Nevertheless, protracted exposure to increased serotonin concentrations can bring about problems like diarrhea, IBD, and the advancement of tumors. As such, firm regulation of serotonin is indispensable for upholding a healthy gut.
Within the mice, a deficiency in sleep not only prompted an overflow of serotonin discharged by the intestinal cells, but also diminished “reuptake” of the molecule — which led to a progressive accumulation of the chemical messenger within the gut. When the research group attempted to inject serotonin into the guts of fully rested mice, they noted alterations akin to those induced by sleep deprivation.
You may like
-

Initial studies suggest reasons for why women undergo sharper gut pain than men
-
Early study suggests that eliminating ‘zombie cells’ inside blood vessels could be vital to treating diabetes
-
‘Mitochondrial transfer’ into nerves could relieve chronic pain, early study hints
But precisely through what mechanism do the brain signals connected to poor sleep conditions influence the gut? Yu and fellow researchers speculated that the vagus nerve, responsible for overseeing gut-brain interaction during periods of stress, might serve as this connection.
To assess this conjecture, the researchers scrutinized the consequence of sleep deprivation within mice that were subjected to vagus nerve severance. These test animals sustained standard serotonin concentrations alongside a greater tally of intestinal stem cells as opposed to sleep-deprived counterparts featuring intact vagus nerves. Hindering vagus-nerve signals similarly sheltered the gut from the ramifications of disordered sleep. The investigation team also singled out acetylcholine as being the preeminent signaling molecule emitted from the vagus nerve, which sets off serotonin release.
RELATED STORIES
—A new investigation begins to decipher why insomnia and anxiety accompany a weakened immune response
—A primary regulator of inflammation has been discovered — and resides inside the brain stem
—Gut bacteria that inflict DNA damage might bolster colon cancer progression amongst patients with inflammatory bowel ailment
“Each individual component in this process is distinctly crucial as a possible target for therapies,” voiced Maksim Plikus, a cell biologist at the University of California, Irvine, who also contributed to the investigation, in comments to Live Science. Further down the line, the team aspires to scrutinize the process inside scaled-down replicas of the gut, known as organoids.
“We must shift our focus towards human intestinal organoids so we can commence with verifying the preservation status of cell types and neural networks,” Plikus declared.
Currently, Yu and the team are examining the relevance of this pathway in the context of continual sleep disorders to confirm whether the prolonged activation of the vagus nerve has the potential to contribute to the development of cancerous growths or IBD. Eventually, the intention is to formulate therapies targeting the vagus nerve or associated molecular pathways, in a move to address gut malfunction within insomnia patients.
Disclaimer
This article is for informational purposes only and is not meant to offer medical advice.
Article Sources
Zhang, M., et al. (2026). Sleep disturbance triggers aberrant activation of vagus circuitry and induces intestinal stem cell dysfunction. Cell Stem Cell, 33(2), 306-324.e8. https://doi.org/10.1016/j.stem.2026.01.002
Sleep quiz: How much do you know about sleep and dreams?

Sahana SitaramanScience writer
Sahana Sitaraman functions as a science writer based in Lausanne, Switzerland, with biology being her field of expertise. She finds particular delight in writing about unusual animal behavior and its underpinning neuroscience, psychological well-being, and the engagement of women in STEM domains. She also tries her hand at creating illustrations for standout discoveries that hold her attention. Sahana, during her own time, can be found either embarking on a nature hike, acting with a local improv group, or engaged in a painting project. She holds a bachelor’s qualification in microbiology obtained from the University of Delhi, India, in addition to a master’s qualification plus a PhD in life sciences secured from the National Centre for Biological Sciences situated in Bangalore, India.
View More
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
LogoutRead more

Initial studies suggest reasons for why women undergo sharper gut pain than men
Early study suggests that eliminating ‘zombie cells’ inside blood vessels could be vital to treating diabetes
‘
