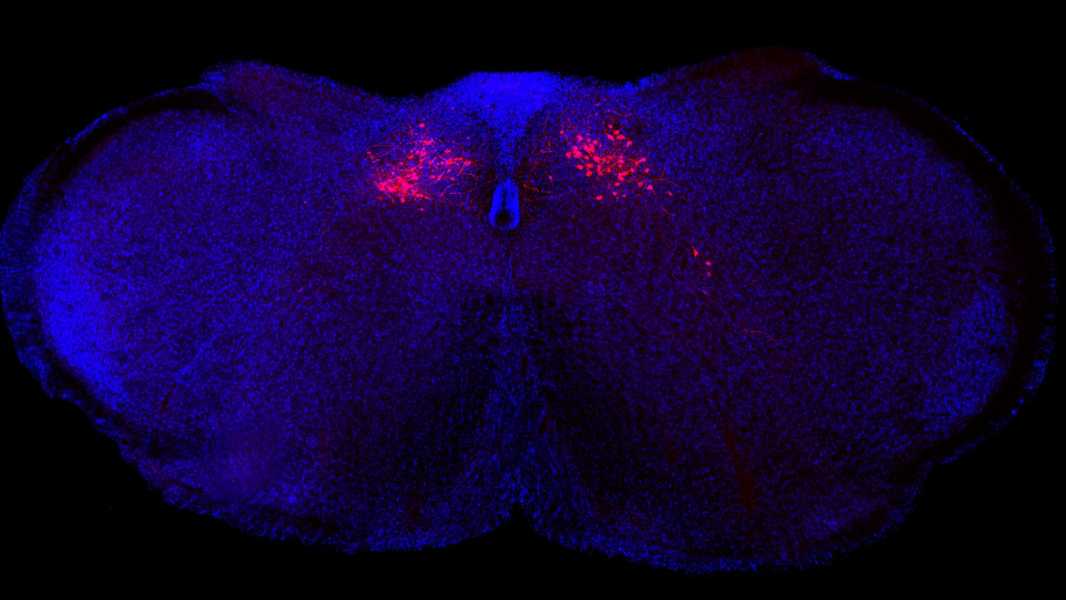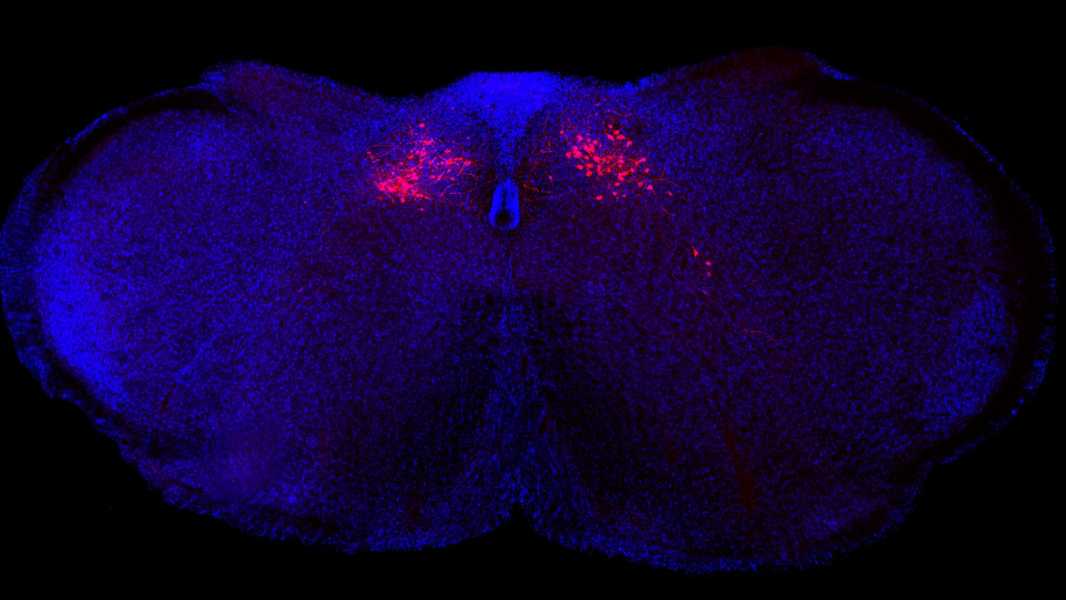
A new study in mice shows that inflammation is controlled by neurons (red in the image above) in the brainstem. (Image credit: Columbia Zuckerman Institute)
Scientists have identified a key regulator of the inflammatory process – it is located in the brainstem.
A new study in mice has found that neurons in the brainstem function like a thermostat, increasing or decreasing inflammation in response to signals from the vagus nerve, which connects the brain to other organs in the body.
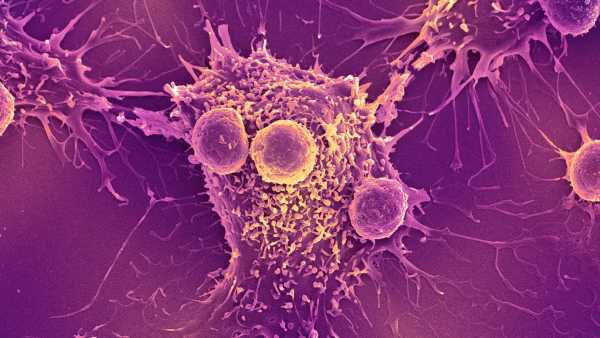
Early in an infection, these neurons can activate a helpful proinflammatory response to prevent pathogens from invading. However, once the infection is cleared, the neurons suppress this response to avoid causing unnecessary damage to healthy cells. The researchers described this feedback loop in a new study published May 1 in the journal Nature.
If a similar feedback system is discovered in humans, scientists may one day be able to create drugs that regulate it. For example, drugs that target this brainstem thermostat could be used to reduce inflammation in conditions where it malfunctions, such as autoimmune disorders, the researchers say.
“If we can engineer small molecules that get into these neurons and activate them, then we have a way to regulate the circuit and therefore change how they modulate the body’s immune response and inflammatory state,” Charles Zucker, who led the lab where the study was conducted and is a professor of biochemistry, molecular biophysics, and neuroscience at Columbia University, told Live Science.
The brain stem connects the main part of the brain, the cerebrum, to the cerebellum and spinal cord, and it regulates important involuntary functions such as breathing and heart rate. Researchers already knew that the brain and immune system interact closely with each other, but the brain stem’s role in this relationship remained unclear.
Scientists also knew that the vagus nerve plays an important role in inflammation; stimulating it has been shown to be effective in a variety of inflammatory conditions, including inflammatory bowel disease (IBD) and rheumatoid arthritis. However, exactly how all these components interact was unclear.
To explore this connection, in the new study, Zucker and his colleagues induced an infection in mice using bacterial molecules that typically trigger an inflammatory response.
These molecules activate the vagus nerve, causing it to send signals to neurons in the caudal nucleus of the solitary tract (cNST) in the brainstem.
In a separate experiment, suppressing the activity of cNST neurons led to an enhanced inflammatory response, causing the body to produce three times more pro-inflammatory molecules and three times fewer anti-inflammatory molecules than normal levels in healthy mice.
Stimulating these neurons, in contrast, had the opposite effect — levels of pro-inflammatory molecules dropped by nearly 70%, while anti-inflammatory molecules increased nearly 10-fold. This suggests that cNST neurons may control the body's inflammatory response to infection, the team said.
Despite these encouraging preliminary results, many questions remain. For example, more research will be needed to understand what signals are transmitted from the brainstem to immune cells elsewhere in the body, Tamar Ben Shaanan, a postdoctoral researcher in microbiology and immunology at the University of California, San Francisco, who was not involved in the study, told Live Science in an email.
Jonathan Kipnis, a professor of pathology and immunology at Washington University School of Medicine in St. Louis, who was also not involved in the study, stressed the importance of deciphering how the complex immune “picture” plays out in the brain.
For example, future studies could test whether the brain is aware of
Sourse: www.livescience.com