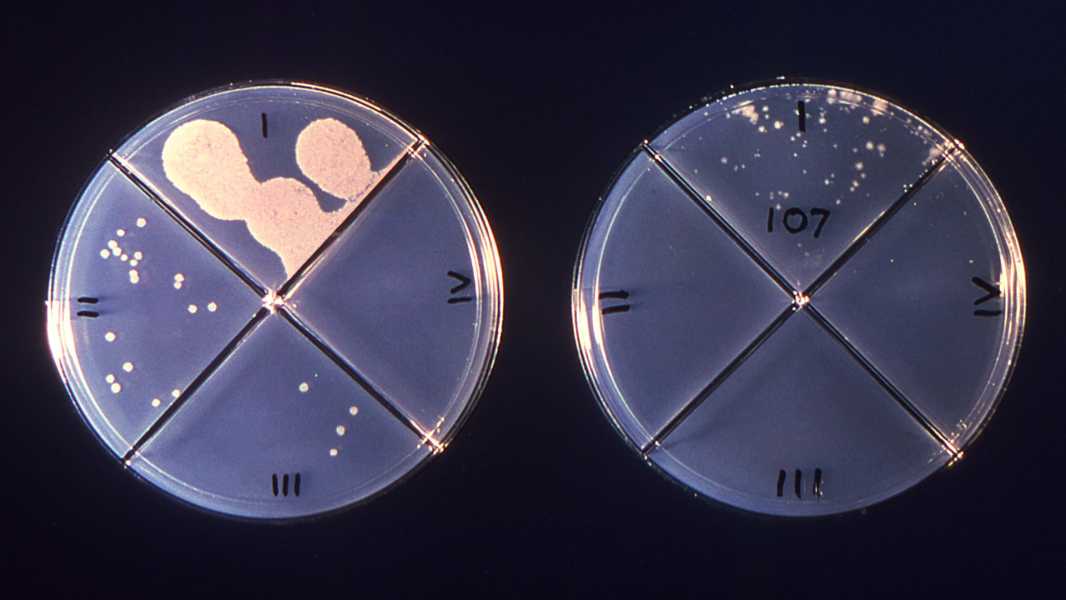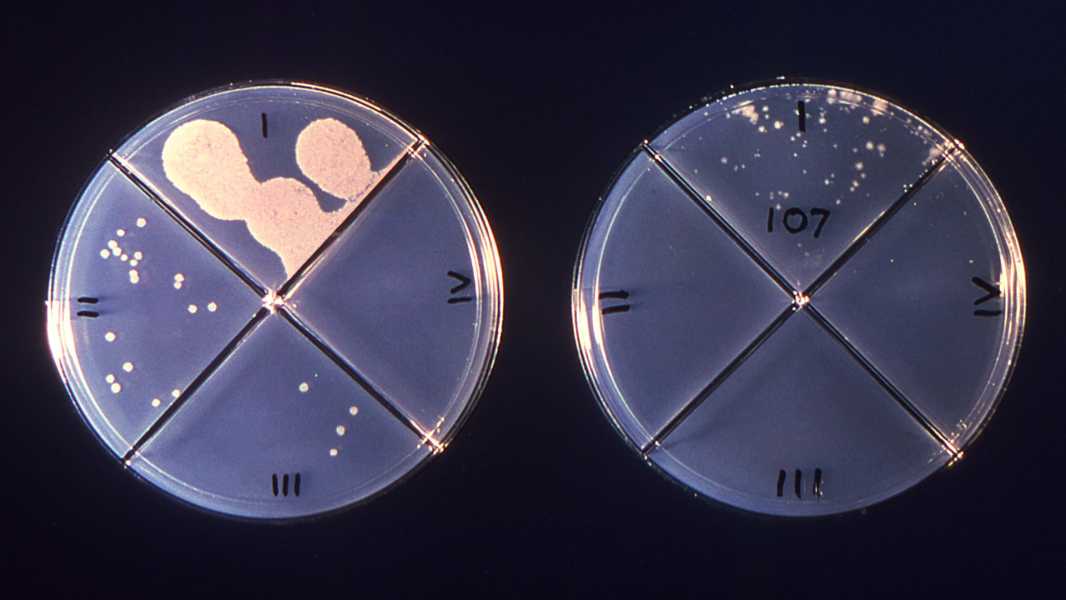
These plates contain Mycobacterium tuberculosis, the bacteria that causes tuberculosis (TB). Each highlighted area contains a different antibiotic, and you can tell which ones the bacteria are resistant to based on how much they grow in that area. Drug resistance makes TB much more difficult to treat. (Image credit: CDC/Dr. George Kubica)
Author John Green has been fascinated by tuberculosis (TB) since 2019, when he first visited Lakka Government Hospital in Sierra Leone and met a young TB patient named Henry Rader. In his latest book, Everything Is Tuberculosis: The History and Persistence of Our Deadliest Infection (Crash Course Books, 2025), Green explores the history of this bacterial disease, highlighting its importance across historical eras. He also focuses on the current reality of TB—a curable disease that nonetheless claims more than a million lives each year due to appalling health inequities around the world.
Today, Green argues that injustice is the primary cause of TB morbidity and mortality, and that we can collectively resolve to address this injustice and finally eradicate this deadly disease.
At the time, I knew almost nothing about tuberculosis. To me, it was a disease of the past – something that took the lives of depressed 19th-century poets, not modern people. But as a friend once told me, “There is nothing more privileged than to think that history belongs to the past.”
When we arrived in Lakka, we were immediately greeted by a child who introduced himself as Henry. “That’s my son’s name,” I told him, and he smiled. Most Sierra Leoneans speak several languages, but Henry spoke English particularly well, which allowed us to carry on a conversation beyond my few halting phrases in Krio. I asked him how he was, and he replied, “I’m happy, sir. I’m inspired.” He loved that word. Who wouldn’t? Inspiration, like courage, is something we strive for in ourselves and inspire in others.
My son Henry was 9 years old at the time, and this Henry looked about the same age, a small boy with thin legs and a wide, easygoing smile. He was wearing shorts and a loose rugby shirt that came almost to his knees. Henry grabbed my shirt and started leading me around the hospital. He showed me a lab where a technician was looking through a microscope. Henry peered through the microscope too, and then asked me to come in because the technician, a young woman from Freetown, had explained that the sample contained tuberculosis, even though the patient had been on standard therapy for months. The technician started to tell me about “standard therapy,” but Henry tugged at my shirt again. He led me through the wards, a complex of poorly ventilated buildings containing hospital rooms with barred windows, thin mattresses, and no toilets. The rooms had no electricity or running water. To me, the rooms looked like prison cells. Before it became a tuberculosis hospital, Lakka was a leper ward – and it looked like one.
Inside each room, one or two patients lay on cots, usually on their sides or backs. Several men sat on the edges of the beds, leaning forward. All of these men (the women were in a separate room) looked emaciated. Some were so weak that their skin seemed to stretch tightly over their bones. As we walked down the hallway between the buildings, Henry and I watched as a young man drank water from a plastic bottle and then immediately vomited a mixture of bile and blood. I instinctively looked away, but Henry continued to stare at the man.
I thought,
Sourse: www.livescience.com