
(Image credit: Justin Paget via Getty Images)
Like lots of fresh mothers, Lisette Lopez-Rose anticipated that the arrival of her child would introduce a happy period. Instead, she was experiencing anxiety attacks, thinking something terrible might befall her infant, and she felt oppressed by a gloom she couldn’t shake off. The mom from the San Francisco Bay vicinity realized her intense feelings weren’t usual, yet she hesitated to share with her physician. What if they took her child from her?
Around the time her baby was six months old, she found an internet community of women with comparable circumstances and ultimately confided in her general doctor. “Approximately a couple of months after commencing medication, I began to feel like I was rising from a dark pit and observing light once more,” she recounts. Currently, Lopez-Rose is employed at Postpartum Support International, organizing volunteers in order to assist new mothers in building online friendships.
You may like
-

FDA panel has cast doubt on whether antidepressants are safe in pregnancy. Here’s what the science actually says.
-

Even brief exposure to air pollution can push the placenta into an inflammatory state, lab study suggests
-

Don’t use cannabis during pregnancy or breastfeeding, leading OBGYN group says
The first-of-its-kind medication for postnatal depression, which has a derivative of progesterone, was given clearance by the US Food and Drug Administration back in 2019. That signaled a fresh perspective to addressing the ailment. This approaching winter, in a different considerable advancement, a startup firm located in San Diego is scheduled to roll out a blood analysis capable of anticipating a pregnant woman’s likelihood of acquiring postnatal depression with an accuracy higher than 80 percent.
The offering, dubbed myLuma, stands to be the initial commercially accessible assessment leveraging biomarkers — biological molecules present within the body, specifically the blood in this scenario — for the purpose of forecasting the emergence of a mental health condition. This methodology mirrors how blood tests are employed to identify indications of conditions like cancer and diabetes. Expectant mothers who are informed of their increased susceptibility to postnatal depression could take preventative measures. These may include using antidepressants subsequent to giving birth or arranging for added assistance.
According to Jennifer Payne, a reproductive psychiatrist operating at the University of Virginia situated in Charlottesville and a leading researcher engaged in the investigations resulting in the fresh test, a blood analysis may alleviate the societal judgment that prevents numerous women from pursuing assistance. She serves as a founder and is a part of the scientific advisory committee for Dionysus Health, the company manufacturing myLuma.
“If we have a blood test, it simplifies psychiatry down to the realm of biology, something that the typical individual might grasp as a condition demanding care and not merely a figment of one’s imagination,” she remarks.
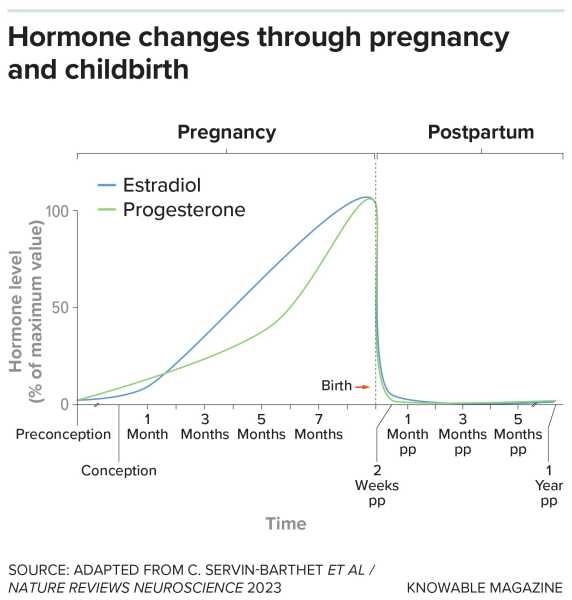
During pregnancy, the levels of estradiol (the predominant form of estrogen) and progesterone surge. In particular women, their abrupt decline following childbirth precipitates the beginning of postnatal depression. Unpredictable effects of hormones
Payne participated as a fellow at the National Institute of Mental Health in 2001, where she was captivated by postnatal depression as a potential glimpse into the genesis of mood disorders. This curiosity led her to a crucial question: Why does the sudden reduction in hormones in the aftermath of childbirth considerably affect some women but not others? While it’s not uncommon for women to undergo fleeting bouts of worry and melancholy within days of delivery, only a segment experiences a more profound and enduring depression.

Lisette Lopez-Rose triumphed over her postnatal depression and presently aids in coordinating support groups via Postpartum Support International. She and her daughter, who is now 4 years old, are doing very well.
During the progression of Payne’s investigations, she joined forces with Zachary Kaminsky, who at the time, was a fellow worker at Johns Hopkins University and was researching the impact of estrogen on the brains of mice. Kaminsky is a specialist in epigenetics, meaning he examines how minuscule chemicals referred to as methyl groups can fasten to genes and sway their level of activity. Ecological elements spanning from pollution to sustenance have the capacity to influence the magnitude of this reversible methylation.
Through contrasting female mice given elevated quantities of estrogen with those lacking it, Kaminsky made the discovery that estrogen instigated specific gene methylation patterns within the cells of the hippocampus, a cerebral region instrumental in regulating mood. These outcomes proposed potential indicators to seek in blood specimens Payne gathered from 51 women with a background of mood disturbances. These women had been monitored consistently throughout their pregnancies and beyond, with some experiencing postnatal depression in the four weeks after childbirth.
You may like
-

FDA panel has cast doubt on whether antidepressants are safe in pregnancy. Here’s what the science actually says.
-

Even brief exposure to air pollution can push the placenta into an inflammatory state, lab study suggests
-

Don’t use cannabis during pregnancy or breastfeeding, leading OBGYN group says
From the research, a pair of estrogen-responsive genes arose: HP1BP3 and TTC9B. Above 80 percent of the women impacted by postnatal depression exhibited a distinct pattern involving heightened methylation in one gene and reduced methylation in the other. Further emphasizing this, the transformations in these genes were identifiable throughout all three trimesters of pregnancy, according to Kaminsky, presently with the University of Ottawa Institute of Mental Health Research at the Royal; he also shares the role of cofounder at Dionysus. In essence, Kaminsky suggests that as early as the onset of pregnancy, “you can foresee which women are liable to experience postnatal depression.”
Kaminsky, Payne, and their associates have verified these results on numerous occasions. As documented in a 2016 publication in Neuropharmacology, their research indicated that, by analyzing the methylation patterns of these genes, they could precisely anticipate above 80 percent of postnatal depression occurrences among 240 expectant women devoid of prior psychiatric conditions. In another cooperative effort published in 2020 in Psychiatry Research, researchers hailing from Johns Hopkins, Emory University, and the University of California, Irvine, including both Payne and Kaminsky, assessed blood samples obtained from 285 expectant women and equally corroborated the conclusions.
That epigenetic investigation constitutes the foundation of the myLuma assessment, which likewise integrates supplementary biomarkers to augment its precision, as mentioned by Kaminsky. Commencing in January 2026, availability is projected at selected physicians’ offices across three states: Florida, Texas, and California. Even though it is not yet endorsed by the FDA, clinicians have the authorization to employ such lab examinations to assist them in rendering clinical judgments.
Zeroing in on steroids
Not everyone afflicted by postnatal depression possesses these epigenetic alterations, which motivates Payne and other scientists to persistently search for further biomarkers so as to gain insight into how hormonal shifts prompt postnatal depression. For instance, they are concentrating particularly on neuroactive steroids, which are naturally produced by the body utilizing molecules akin to progesterone within the brain and other bodily tissues.
Among these metabolites, allopregnanolone has a soothing influence, functioning by affecting a receptor site in the brain recognized as GABA-A, which is well documented for its role in diminishing stress. The level of allopregnanolone increases as pregnancy advances and then diminishes swiftly subsequent to delivery. An additional neuroactive steroid, pregnanolone, shares comparable attributes. On the other hand, isoallopregnanolone diminishes the antidepressant actions of allopregnanolone, leading to amplified feelings of unease.
Within a research project encompassing 136 pregnant participants and published in 2025 within the journal Neuropsychopharmacology, females exhibiting an imbalance between pregnanolone and isoallopregnanolone throughout gestation displayed a greater inclination to experience postnatal depression. According to Lauren M. Osborne, a reproductive psychiatrist linked to Weill Cornell Medicine situated in New York City and co-leader of the research initiative alongside Payne, evaluating the proportion of these chemicals within the bloodstream might present a distinct approach to forecasting postnatal depression.
Concurrently, allopregnanolone has already shown its worth as a beneficial instrument for intervention. A synthetic variant identified as brexanolone was created through Cambridge, Massachusetts-located Sage Therapeutics and secured FDA endorsement back in 2019, marking it as the primary pharmaceutical specifically endorsed for postnatal depression. Initially delivered through IV infusion, its utilization has been supplanted by an oral form, zuranolone, which was granted FDA approval in 2023.
If we have a blood test, it simplifies psychiatry down to the realm of biology, something that the typical individual might grasp as a condition demanding care and not merely a figment of one’s imagination.
Jennifer Payne, University of Virginia in Charlottesville
As stated by the authors of a 2025 document featured within the Annual Review of Medicine, these are regarded as “transformative therapies” due to their expedited effectiveness. Samantha Meltzer-Brody, a reproductive psychiatrist associated with the University of North Carolina and the coauthor of the article, along with being an academic principal investigator involved in studies on brexanolone and an investigator in trials pertaining to zuranolone, suggests that females exhibiting elevated susceptibility to postnatal depression might even reap advantages from taking zuranolone preventatively, even though such a method remains untested.
She further adds that the accessibility of a blood examination “initiates an entirely different scope of questioning concerning the means to remain ahead of it, eliminating the requirement to await the initiation of suffering.”
Furthermore, prospects for a postnatal depression assessment exist. In a 2022 article published in Molecular Psychiatry, Sarven Sabunciyan, a neuroscientist from Johns Hopkins, along with Osborne, Payne, and Morgan Sherer, who was an immunologist at Johns Hopkins during that time, delineated a limited study revealing variations in the types of RNA transported through blood in fatty encapsulations among females who developed postnatal depression, both throughout pregnancy and thereafter. Specifically, a decrease was observed in RNA variants associated with autophagy, which entails the elimination of debris from cells. Autophagy has been correlated with other psychiatric conditions.
Another prospective avenue involves Eynav Accortt, a clinical psychologist specializing in perinatal mental wellness based at Cedars-Sinai Medical Center in Los Angeles, who identified an arrangement of changed proteins within plasma specimens acquired from females who developed perinatal mood and anxiety disturbances, which constitute a cluster of conditions inclusive of postnatal depression. This encompassed proteins contributing to neuron operation and inflammation, an element recognized for its implication in depression.
While researchers persist in investigating these probabilities, Payne is overseeing a broad clinical analysis that will furnish richer specifics concerning the predictive worth of the myLuma assessment. As an illustration, the investigation will delve into the proportions of false positives (females classified as susceptible but not exhibiting postnatal depression) and false negatives (females experiencing postnatal depression yet not flagged by the assessment). This constitutes a vital move toward acquiring FDA authorization, which could render the assessment explicitly accessible to expectant mothers.
RELATED STORIES
—Dangers of falling birth rates in the US have been ‘dramatically overstated,’ experts say
—’Pregnancy robot from China’ is fake, but is the technology behind it possible?
—’We know what to do; we just have to implement it.’: Pregnancy is deadlier in the US than in other wealthy countries. But we could fix that.
Lopez-Rose recalls the intensity of fear she felt in the months subsequent to her daughter’s birth. During those trying occasions, she left her employment, obtained minimal sleep, and was inundated with unfavorable thoughts. She had many feelings of uncertainty about herself, but she now comprehends that seeking support was reflective of her capabilities as a devoted mother.
At present, her daughter is four years in age and is flourishing, mirroring the condition of Lopez-Rose. Still, she indicates that a blood assessment would have advised her on indicators to anticipate, “instead of it being so startling as I underwent my depression.”
This article originally appeared in Knowable Magazine, a nonprofit publication dedicated to making scientific knowledge accessible to all. Sign up for Knowable Magazine’s newsletter.
Michele Cohen MarillJournalist
Michele Cohen Marill is a freelance writer based in Atlanta. Her work has appeared in MindSite News, Health Affairs, WIRED.com, WebMD, STAT and Kaiser Health News. She is a board member of Association of Health Care Journalists (AHCJ ) and received a 2020 AHCJ Health Study Fellowship.
You must confirm your public display name before commenting
Please logout and then login again, you will then be prompted to enter your display name.
LogoutRead more

FDA panel has cast doubt on whether antidepressants are safe in pregnancy. Here’s what the science actually says.

Even brief exposure to air pollution can push the placenta into an inflammatory state, lab study suggests

Don’t use cannabis during pregnancy or breastfeeding, leading OBGYN group says
Sourse: www.livescience.com





